"This is a very bold goal, but we have decided to go big," Dr. Francis Collins, director of the NIH, said in a news conference today.
The effort aims to have the therapies ready for testing in clinical trials in the U.S. and sub-Saharan Africa within the next seven to 10 years.
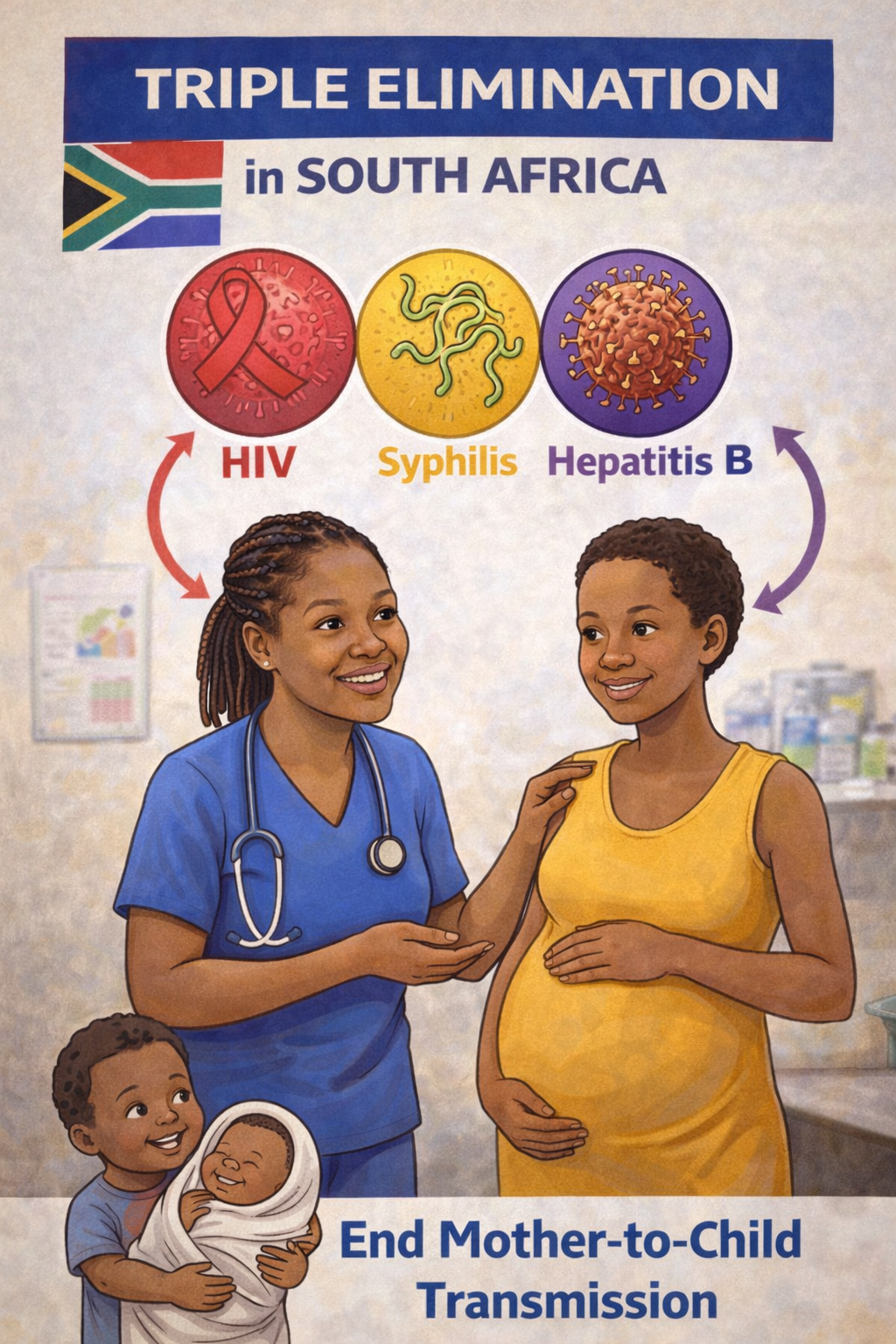
The majority of the 38 million people with HIV live in developing countries, with two-thirds living in Sub-Saharan Africa. For sickle cell disease, the majority of cases also occur in Sub-Saharan Africa.
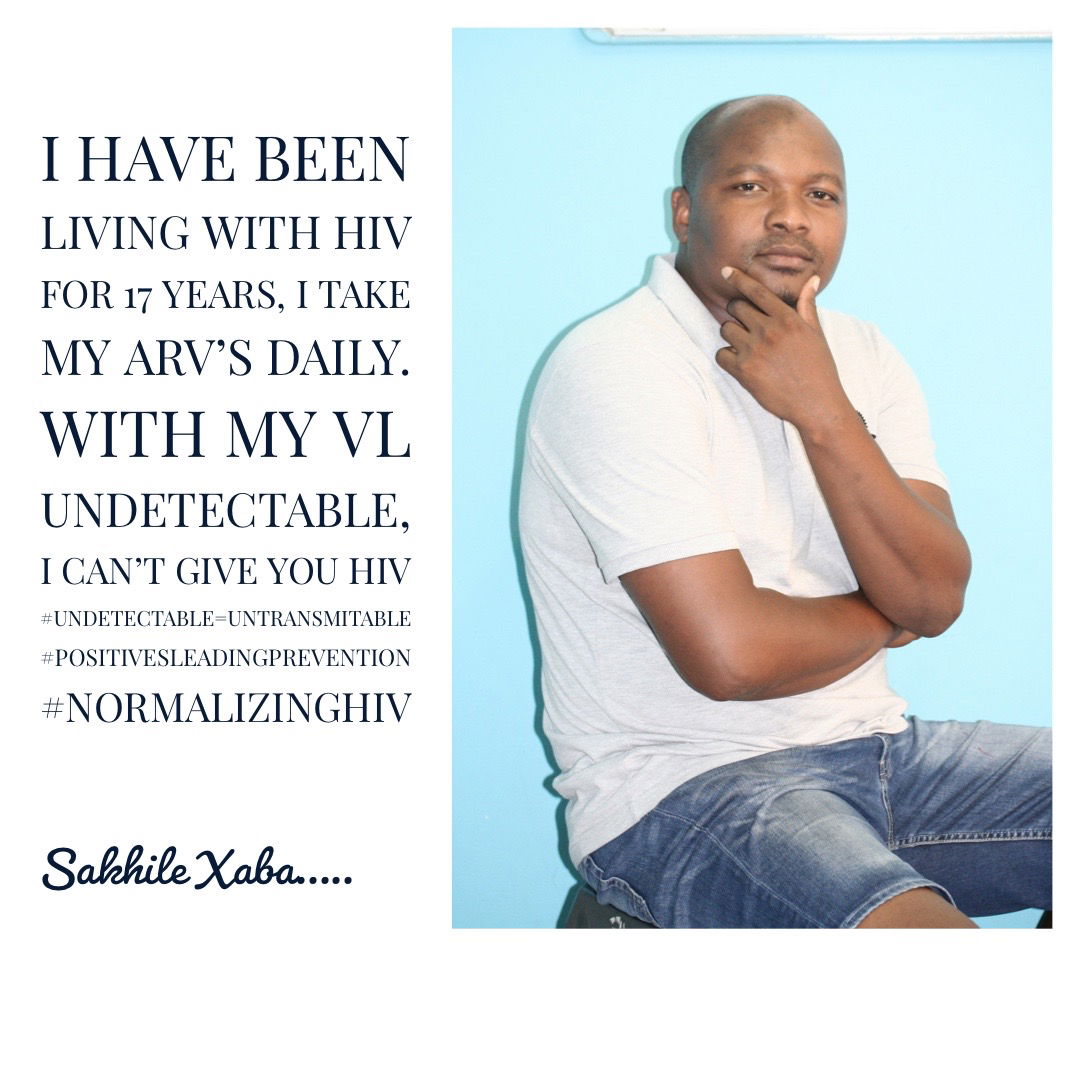
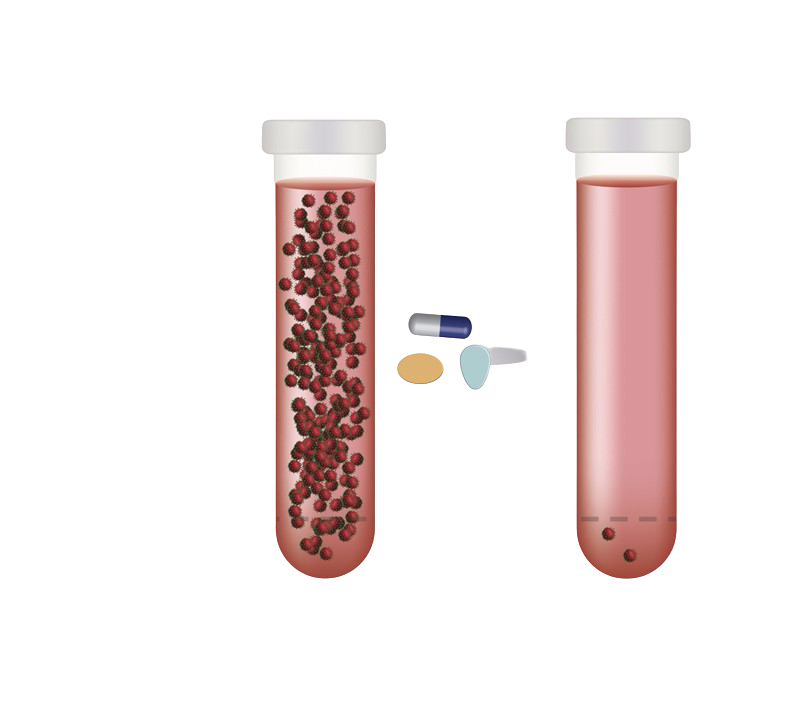
The NIH has been trying to find a cure for HIV for "decades and decades," said Dr. Anthony Fauci, director of The National Institute of Allergy and Infectious Diseases. Although current treatments with antiretroviral therapy (ART) are effective at suppressing the virus in the body, they are not a cure, and must be taken everyday. What's more, there are millions of people with HIV who don't have access to ART treatment.
Although scientists are working to develop gene-based cures for HIV, these approaches are often costly and would be difficult to implement on a large scale, Fauci said. For example, some of these therapies take cells out of a patient's body and then re-infuse them, an expensive and time-consuming intervention.
For this reason, the new collaboration will focus on developing cures that use "in vivo" approaches, meaning they happen inside the body, Fauci said. One example of this could be to remove the gene for the CCR5 receptor, which HIV uses to get inside cells. Another idea is to excise the HIV "proviral" DNA that has copied itself into the human genome and lurks in the body even after years of treatment.
Similarly, for sickle cell disease, the goal would be to develop an in vivo therapy that could repair the genetic mutation that causes the disease. This would require a gene-based delivery system that could selectively target the mutation.
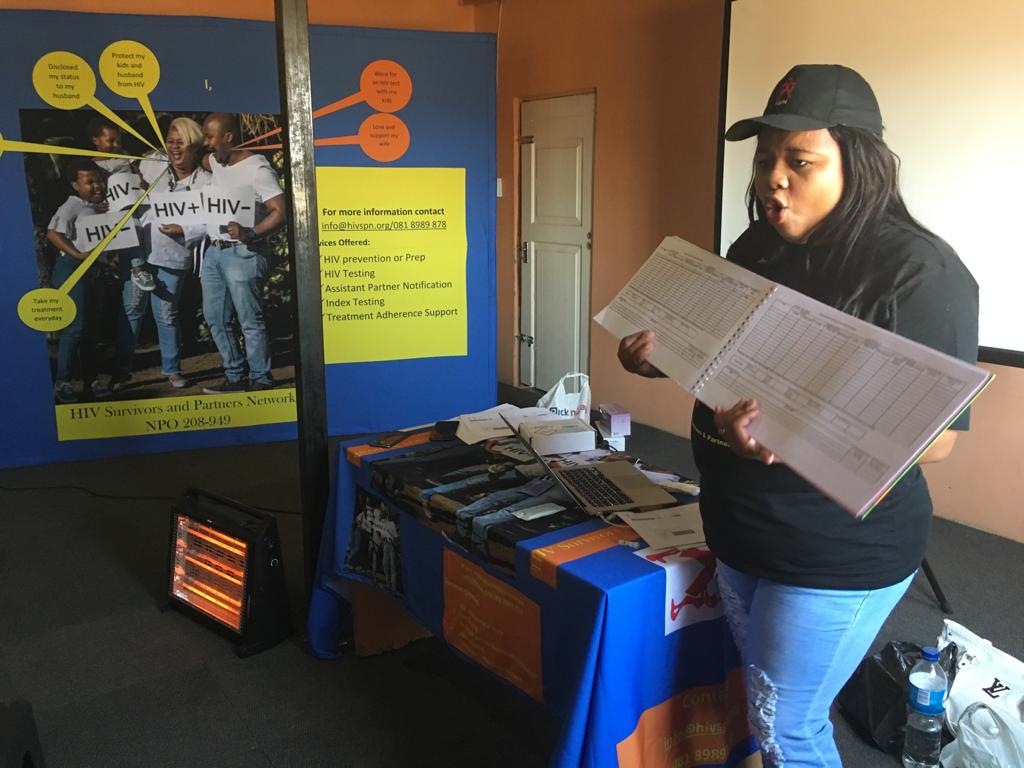
"Beating these diseases will take new thinking and long-term commitment. I'm very pleased to see the innovative collaboration announced today, which has a chance to help tackle two of Africa's greatest public health challenges," Matshidiso Rebecca Moeti, the World Health Organization's Regional Director for Africa, said in a statement.
Still, much work would be needed to make sure these therapies are safe and effective.
"It is very clear we have a ways to go, which is why this is a 10 year effort to try and take that promise and turn it into a reality," Collins said.
Earlier this year, the Trump Administration announced a plan to end the HIV epidemic in the U.S. in 10 years.